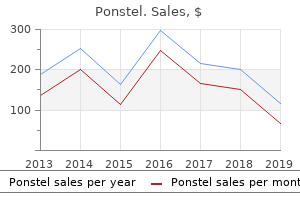
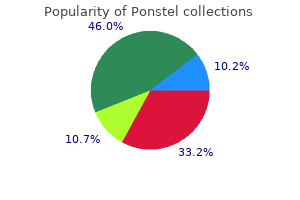
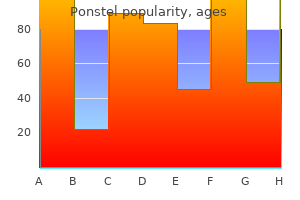
Buy ponstel in united states onlineThe higher boundary is shaped by the weak hyoepiglottic membrane spasms the movie trusted ponstel 250 mg, strengthened medially as the median hyoepiglottic ligament; the anterior boundary is the thyrohyoid membrane spasmus nutans treatment cheap ponstel 500 mg without prescription, strengthened medially because the median thyrohyoid ligament; and the decrease boundary is the thyroepiglottic ligament muscle relaxant tinidazole order ponstel 250 mg on-line, continuous laterally with the quadrangular membrane behind spasms foot trusted 500 mg ponstel. It is also in continuity with the mucosa of the laryngeal surface of the epiglottis by way of multiple perforations within the cartilage of the epiglottis (Reidenbach 1996a). At rest, the upper border of the infant epiglottis is on the degree of the second or third cervical vertebra; when the larynx is elevated, it reaches the extent of the primary cervical vertebra. This excessive place allows an infant to use its nasal airway to breathe whereas suckling. The epiglottis is X-shaped, with a furled petiole, and the laryngeal cartilages are softer and more pliable than in the adult larynx (which may predispose to airway collapse in inspiration, leading to the medical picture of laryngomalacia). The thyroid cartilage is shorter and broader, and lies closer to the hyoid bone in the neonate, which means that the thyrohyoid ligament is comparatively brief. Calcification of the cricoid cartilage has been noted as early as 7 years of age (Strauss 2000). The arytenoid cartilages are larger in proportion to the larynx as a whole and so are extra outstanding; the aryepiglottic folds are disproportionally large. The time at which the infant larynx assumes grownup characteristics varies in the literature from 5 to 12 years; some adults retain a funnelshaped larynx (Wheeler et al 2009). Further discussion is beyond the scope of this guide; the interested reader should consult Wheeler et al (2009) and Holzki et al (2010). The mucosa can be lax in the infraglottic cavity and swelling here quickly causes severe respiratory obstruction due to the disproportionally narrower lumen (3. The neonatal infraglottic cavity extends posteriorly in addition to inferiorly, which is a crucial consideration when passing an endotracheal tube (Litman et al 2003). The infraglottic airway quickly will increase in size through the first two years of life (Eckel et al 1999). By concerning the third 12 months, sexual variations turn out to be obvious: the larynx is larger in boys, although the angle between the thyroid laminae is more pronounced in girls. Congenital anomalies of the larynx embody aplasia and hypoplasia of the epiglottis, high-rising epiglottis, bifid epiglottis, saccular cysts, vocal wire palsy, laryngeal atresia, laryngocele, laryngo-tracheooesophageal cleft and laryngeal net. It is bounded laterally by the thyroid cartilage and thyrohyoid membrane, superomedially by the quadrangular membrane, inferomedially by the conus elasticus, and posteriorly by the piriform fossa. The lower border of the thyroid cartilage is inferior, and the paraglottic house is continuous inferiorly with the house between the cricoid and thyroid cartilages. Anteroinferiorly, there are deficiencies in the paramedian gap in conjunction with the median cricothyroid ligament, and posteroinferiorly, adipose tissue extends in path of the cricothyroid joint. Superiorly, the paraglottic house is usually continuous with the pre-epiglottic house, although the two spaces could also be separated by a fibrous septum. There is disagreement between authors as to the precise boundaries between these two spaces. Some authorities exclude thyroarytenoid from the paraglottic space and include it inside the preepiglottic area, forming its inferior border posterolaterally (Reidenbach 1996b). It is continuous below with the internal surface of the cricoid cartilage and its mucosa (Reidenbach 1998). The extrinsic muscular tissues join the larynx to neighbouring structures and are liable for moving it vertically during phonation and swallowing. They embrace the infrahyoid strap muscles, thyrohyoid, sternothyroid and sternohyoid, and the inferior constrictor muscle of the pharynx. The position of the extrinsic muscle tissue throughout respiration seems to be variable; the larynx has been seen to rise, descend or barely transfer during inspiration. The extrinsic muscles can affect the pitch and the quality of the voice by raising or reducing the larynx, and geniohyoid elevates and anteriorly displaces the larynx, notably throughout deglutition. Elevation of the larynx decreases the size and calibre of the laryngopharynx and thus shortens the vocal tract general. The raising of the larynx may also be accompanied by ahead or backward motion of the tongue due to the attachment of the tongue to the hyoid bone. Another impact of lowering the larynx might be to decrease supraglottal pressure and this can facilitate the articulation of voiced stops and fricatives (to a lesser extent). Voice quality can also be varied by the height of the larynx and this is a crucial issue contributing to the variations in high quality of voice between different speakers. Whereas most of the intrinsic muscles lie internally, underneath cowl of the thyroid cartilage or the mucosa, the cricothyroids seem on the outer aspect of the larynx.
Buy 250 mg ponstelInfec tion muscle relaxant for migraine cheap ponstel amex, malignancy and postoperative inflammation of the tonsil and tonsillar fossa may therefore be accompanied by pain referred to the ear spasms pain rib cage order online ponstel. Tonsillectomy Surgical elimination of the pharyngeal tonsils is commonly performed to prevent recurrent acute tonsillitis or to treat airway obstruction by hypertrophied or inflamed palatine tonsils spasms vs fasciculations generic 250 mg ponstel visa. Occasionally muscle relaxant for joint pain order ponstel 250mg with mastercard, the tonsil may be eliminated to deal with an acute peritonsillar abscess, which is a collection of pus between the superior constrictor and the tonsillar hemicapsule. Many methods have been employed, the commonest being dissec tion within the airplane of the fibrous hemicapsule, adopted by ligation or electrocautery to the vessels divided in the course of the dissection. The nerve supply to the tonsil is so diffuse that tonsillectomy beneath local anaes thesia is carried out efficiently by native infiltration rather than by blocking the primary nerves. Surgical entry to the glossopharyngeal nerve could additionally be achieved by separating the fibres of superior constrictor. It is made up anteroinferiorly by the lingual tonsil, laterally by the palatine and tubal tonsils, and posterosuperiorly by the pharyn geal tonsil and smaller collections of lymphoid tissue in the intertonsil lar intervals. The laryngeal inlet lies in the upper part of its incomplete anterior wall, and the posterior surfaces of the arytenoid and cricoid cartilages lie below this opening. The largest is the tonsillar artery, which is a department of the facial, or typically the ascending palatine, artery. It ascends between medial pterygoid and styloglossus, perforates the su perior constrictor at the higher border of styloglossus, and ramifies within the tonsil and posterior lingual musculature. The other arteries found on the lower pole are the dorsal lingual branches of the lingual artery, which enter anteriorly, and a department from the ascending palatine artery, which enters posteriorly to provide the lower part of the palatine tonsil. The higher pole of the tonsil additionally receives branches from the ascending pharyngeal artery, which enter the tonsil posteriorly, and from the descending palatine artery and its branches, the greater and lesser pala tine arteries. All of these arteries enter the deep floor of the tonsil, department within the connective tissue septa, slim to turn into arterioles and then give off capillary loops into the follicles, interfollicular areas and the cavities inside the base of the reticulated epithelium. The capil laries rejoin to type venules, many with excessive endothelia, and the veins return throughout the septal tissues to the hemicapsule as tributaries of the pharyngeal drainage. The tonsillar artery and its venae comitantes typically lie throughout the palatoglossal fold, and should haemorrhage if this fold is damaged during surgical procedure. Instead, dense plexuses of nice lymphatic vessels encompass each follicle and form efferent lymphatics, which cross towards the hemicapsule, pierce the superior constrictor, and drain to the upper deep cervical lymph nodes directly (especially the jugulo digastric nodes) or not directly by way of the retropharyngeal lymph nodes. The jugulodigastric nodes are sometimes enlarged in tonsillitis, after they project past the anterior border of sternocleidomastoid and are palpable superficially 1�2 cm below the angle of the mandible; when enlarged, they symbolize the most common swelling in the neck. Piriform fossa A small piriform fossa lies on each side of the laryn geal inlet, bounded medially by the aryepiglottic fold and laterally by the thyroid cartilage and thyrohyoid membrane. At relaxation, the laryngopharynx extends posteriorly from the lower part of the third cervical vertebral physique to the upper part of the sixth. Below the inlet, the anterior wall of the laryngopharynx is formed by the posterior floor of the cricoid cartilage. It is connected to the basilar a half of the occipital bone and the petrous part of the temporal bone medial to the pharyngotympanic tube, and to the posterior border of the medial pterygoid plate and the pterygomandibular raphe. Inferiorly, it diminishes in thickness however is strengthened posteriorly by a fibrous band hooked up to the pharyngeal tubercle of the occipital bone, which descends because the median pharyngeal raphe of the constrictors. This fibrous layer is actually the internal epimysial covering of the muscles and their aponeurotic attachment to the base of the cranium. These tumours can also give rise to snoring as a result of narrowing of the nasopharynx. Several surgical approaches have been described for the management of parapharyngeal area tumours, including transcervical, transparotid, transcervical�transmandibular and transoral approaches. Transoral robotic surgical procedure uses the oral cavity as a surgical hall; as but, there have been comparatively few studies from the transoral perspective of the relevant surgical anatomy (Dallan et al 2011, Moore et al 2012, Wang et al 2014). The anterior part of the peripharyngeal area is formed by the submandibular and submental spaces, posteriorly by the retropharyngeal house and laterally by the parapharyngeal areas. The retropharyngeal space is an area of loose connective tissue that lies behind the pharynx and anterior to the prevertebral fascia, extending upwards to the base of the skull and downwards to the retrovisceral area within the infrahyoid part of the neck. Each parapharyngeal space passes laterally around the pharynx and is continuous with the retro pharyngeal area. The parapha ryngeal area is divided into an anterior, or prestyloid, compartment and a posterior, or retrostyloid, compartment (Maran et al 1984). The prestyloid compartment contains the retromandibular portion of the parotid gland, fat and lymph nodes.
500mg ponstelThey are strengthened by the nerve provide of the muscle muscle relaxant examples buy ponstel with paypal, and by the relationship between the muscle tissue and certain nerves muscle relaxant norflex order genuine ponstel line. These muscles are homologous with the thoracic intertransverse muscles and ligaments gas spasms discount ponstel 250mg with mastercard. They are homologous with levatores costarum and are provided by the ventral rami of spinal nerves muscle relaxant equipment order on line ponstel. At every stage, the medial branch of a dorsal ramus separates the true intertransverse muscle from levator costae or its equal. They are most distinct in the cervical area, where they encompass six pairs, the primary between the axis and third vertebra, and the last between the seventh cervical and first thoracic vertebrae. In the thoracic region they happen between the primary and second vertebrae (sometimes between the second and third), and the eleventh and twelfth vertebrae. A pair is occasionally found between the final thoracic and first lumbar vertebrae, and one other between the fifth lumbar vertebra and the sacrum. They are very small muscular tissues and are unlikely to be capable of generate enough force to be prime movers of the vertebrae. It due to this fact seems affordable to assume that the quick muscles of the back could serve a proprioceptive operate in controlling the place of the vertebral column and its movements. Rectuscapitisposteriormajor Rectus capitis posterior main is hooked up by a pointed tendon to the backbone of the axis, becomes broader because it ascends, and is attached to the lateral part of the inferior nuchal line and the occipital bone immediately below it. As the muscle tissue of the two sides cross upwards and laterally, they go away between them a triangular area in which components of recti capitis posteriores minores are seen. Rectuscapitisposteriorminor Rectus capitis posterior minor is connected by a narrow pointed tendon to the tubercle on the posterior arch of the atlas. As it ascends, it broadens earlier than attaching to the medial part of the inferior nuchal line and to the occipital bone between the inferior nuchal line and the foramen magnum. There is often a delicate tissue attachment to the posterior atlanto-occipital membrane, which itself is firmly attached anteriorly to the spinal dura in the same area (Zumpano et al 2006). Vascular supply of the true again muscular tissues the true (intrinsic) muscular tissues of the again obtain their blood supply from: the vertebral artery; deep cervical artery; superficial and deep descending branches of the occipital artery; deep department of the transverse cervical artery (when present); superior intercostal artery, by way of dorsal branches of the higher two posterior intercostal arteries; posterior intercostal arteries of the decrease nine areas through dorsal branches; dorsal branches of the subcostal arteries; dorsal branches of the lumbar arteries; dorsal branch of arteria lumbalis ima; and dorsal branches of the lateral sacral arteries. The detailed pattern of the arterial supply of the deep muscles of the again has been described by Michel Salmon (1994). These muscular tissues are supplied by dorsal branches of the posterior intercostal and lumbar arteries. In the thoracic and higher lumbar regions, where the parts of erector spinae run in well-defined longitudinal columns, arterial trunks from these dorsal branches run in the sulci between the columns and between erector spinae and multifidus, giving off branches to provide the muscles. It expands in width as it ascends dorsally, and is hooked up to the occipital bone between the superior and inferior nuchal strains, lateral to semispinalis capitis and overlapping the insertion of rectus capitis posterior major. Laterally, it lies underneath longissimus capitis and typically splenius capitis, both of which overlap obliquus capitis superior. The vertebral artery and the dorsal ramus of the first cervical nerve lie in a groove on the higher floor of the posterior arch of the atlas. VascularsupplyThe suboccipital muscles receive their blood supply from the vertebral artery and deep descending branches of the occipital artery. They lie inferior to the anterior a half of the occipital bone, the place three of the muscle tissue kind the boundaries of the suboccipital triangle: rectus capitis posterior main lies above and medially; obliquus capitis superior lies above and laterally, and obliquus capitis inferior lies under and laterally. With the top in the anatomical place, the suboccipital triangle lies nearly in the horizontal airplane. Axial rotation entails twisting of vertebrae relative to one another with accompanying torsional deformation of intervening discs. Elsewhere in the column, although movement is slight between particular person vertebrae, the range summates to turn into considerable for the column as an entire. In the postcervical column, the effective range of rotation is biggest on the thoracolumbar junction. In the cervical area, the upward inclination of the superior articular facets allows free flexion and extension. The latter is usually higher, and is checked above by locking of the posterior edges of the superior facets of C1 within the occipital condylar fossae, and beneath by slipping of the inferior processes of C7 into grooves inferoposterior to the first thoracic superior articular processes. Flexion stops the place the cervical convexity is straightened, checked by apposition of the projecting decrease lips of vertebral our bodies on subjacent our bodies.
Ponstel 500 mg cheapWhen the pinnacle is sharply rotated in any course spasms thumb joint 250mg ponstel visa, the eyeball rotates by an equal amount in the incorrect way in response to the stimulation of semicircular canal cristae (angular acceleration) ql spasms cheap ponstel master card, and gaze is undisturbed spasms calf muscles cheap generic ponstel canada. Brief rotational actions are commonly combined with translational movements (linear acceleration) which are monitored by otolith organs muscle relaxant injection for back pain 250 mg ponstel for sale. For example, a linear displacement happens in strolling as the head bobs vertically with every stride, and a rotational displacement happens as the pinnacle rolls, invoking otolith and canal responses, respectively, to stabilize the retinal image. The widespread factor for all sorts of horizontal gaze movements is the abducens nucleus. It incorporates motor neurones that innervate the ipsilateral lateral rectus and interneurones that project via the medial longitudinal fasciculus to the contralateral oculomotor nucleus, which controls medial rectus. A lesion of the abducens nucleus leads to a complete lack of ipsilateral horizontal conjugate gaze. A lesion of the medial longitudinal fasciculus produces slowed or absent adduction of the ipsilateral eye, often associated with jerky actions (nystagmus) of the abducting eye, a syndrome referred to as internuclear ophthalmoplegia (Leigh and Zee 2006). The gaze motor command includes specialized areas of the reticular formation of the brainstem, which obtain a selection of supranuclear inputs. The major region for the generation of horizontal saccades is the paramedian pontine reticular formation, located on all sides of the midline in the central paramedian part of the tegmentum, and increasing from the pontomedullary junction to the pontopeduncular junction. Excitatory burst cells make monosynaptic connections with the ipsilateral abducens nucleus. Pause neurones, located in a midline caudal pontine nucleus, called the nucleus raphe interpositus, discharge tonically during fixation but cease firing immediately previous to a saccade. They appear to exert an inhibitory influence on the burst neurones and act as a swap to change from fixation to saccadic mode (Ramat et al 2007). The tonic exercise of neurones in the nucleus prepositus hypoglossi and medial vestibular nucleus is believed to provide a watch place signal to maintain the eccentric position of the attention in opposition to the viscoelastic forces in the orbit. Vestibular nuclei and the perihypoglossal advanced project on to the abducens nuclei. The final common pathway for vertical gaze actions is formed by the oculomotor and trochlear nuclei. The rostral interstitial nucleus of the medial longitudinal fasciculus accommodates excitatory burst neurones that discharge in relation to up-and-down vertical saccadic movements and project to motor neurones involved in vertical gaze. Neurones in and across the interstitial nucleus of Cajal, which lies slightly caudal to the rostral interstitial nucleus of the medial longitudinal fasciculus, present alerts for vertical gaze holding. Lesions inside the posterior commissure predominantly give rise to disturbances in upgaze, associated with other signs of dorsal midbrain syndrome. Discrete lesions placed extra ventrally in the region of the rostral interstitial nucleus of the medial longitudinal fasciculus might trigger blended up-and-down, or primarily downgaze disturbances (Leigh and Zee 2006). The vestibulocerebellum (flocculus and nodule) is concerned in gaze holding, easy pursuit and the vestibuloocular reflex. The dorsal vermis and fastigial nucleus play a serious position in programming accurate saccades and easy pursuit. The cerebral hemispheres are extremely necessary for the programming and coordination of each saccadic and pursuit conjugate eye movements (Ch. There appear to be 4 major cortical areas in the cerebral hemispheres involved in the era of saccades. These are the frontal eye field, which is positioned at the intersection of the superior precentral sulcus with the superior frontal sulcus (Brodmann space 8) (Amiez and Petrides 2009); the supplementary eye subject, which lies in the dorsomedial frontal cortex (Brodmann space 6); the dorsolateral prefrontal cortex, which lies anterior to the frontal eye field in the second frontal gyrus (Brodmann area 46); and a posterior eye subject, which lies within the parietal lobe in the medial wall of the posterior half of the intraparietal sulcus, together with elements of the supramarginal and angular gyri (Brodmann areas 39 and 40), and the adjoining lateral intraparietal sulcus (M�ri et al 1996). These areas all seem to be interconnected and to ship projections to the superior colliculus and the brainstem areas controlling saccades. An anterior system originates in the frontal eye area and projects, both directly and via the superior colliculus, to the brainstem saccadic generators. This pathway also passes indirectly through the basal ganglia to the superior colliculus. Projections from the frontal cortex affect cells within the pars reticularis of the substantia nigra, via a relay within the caudate nucleus.
Quality ponstel 500 mgThe conjunctiva is extra loosely hooked up to underlying tissues over the orbital zone and so folds readily muscle relaxant gel india order ponstel 250mg fast delivery. The bulbar conjunctiva is loosely related to the eyeball over the uncovered sclera muscle relaxant natural generic ponstel 250 mg without prescription, is skinny and transparent spasms head quality ponstel 250 mg, and readily permits the visualization of conjunctival and episcleral blood vessels muscle relaxant vs anti-inflammatory buy cheap ponstel 250mg online. At the free palpebral margins, the conjunctiva is steady with the skin of the eyelids, the liner epithelium of the ducts of the tarsal glands, and with the lacrimal canaliculi and lacrimal sac (see below). The continuity between the conjunctiva and the nasolacrimal duct and nasal mucosa is important in the unfold of an infection. Fornix Orbital Bulbar the conjunctiva is composed of an epithelial layer and an underlying fibrous layer or substantia propria. The form of the epithelium and thickness of the substantia propria range with location. At the margin of the lids, the epithelium is non-keratinized stratified squamous and 10�12 cells thick. The epithelium of the tarsal conjunctiva thins to two or three layers and consists of columnar and flat surface cells. Near the fornices, the cells are taller, and a trilaminar conjunctival epithelium covers much of the bulbar conjunctiva. It thickens nearer to the corneoscleral junction and then adjustments to stratified squamous epithelium typical of the cornea. A proportion of limbal conjunctival epithelial cells function stem cells for the corneal epithelium; this region of the conjunctiva is subsequently important for maintaining corneal integrity. They present a marked regional variation in density, being most frequent in conjunctival areas normally lined by the eyelids, and reduced in quantity within exposed interpalpebral locations (Doughty 2012). The substantia propria, or fibrous layer, is thickest at the fornix and thinnest over the tarsi where conjunctival attachment is firmest. With the exception of the tarsal conjunctiva, the substantia propria adjacent to the epithelium is mainly unfastened. It merges with the fibrous fascia bulbi and episclera within the limbal and bulbar regions, and is loosely hooked up to the sheaths of the recti. Vascular supply and lymphatic drainage Limbal Tarsal Marginal the arteries of the palpebral conjunctiva are derived from the vascular arcades of the eyelids. Many of the small vessels of the eyelid drain to the conjunctival veins, which, in flip, cross back to the orbital and facial veins. A dense capillary community is arranged in a single subepithelial lamina, a distribution that meets the requirement of the cornea throughout sleep, when oxygen is out there to the cornea solely via this vascular system. The bulbar conjunctiva receives blood from the palpebral arcades and from the anterior ciliary arteries that attain the conjunctiva on the orbital floor of the recti. The conjunctiva is innervated by sensory nerves from the identical ophthalmic and maxillary branches of the trigeminal nerve that serve the eyelid. Autonomic nerve fibres are plentiful within the conjunctiva, particularly in bulbar and limbal regions, and are most likely vasomotor in function. It is distributed within the precorneal tear movie (1�2 �l), and alongside the upper and decrease marginal tear strips (5�6 �l), which are wedge-shaped menisci that run alongside the posterior border of the lid margins and be part of collectively at the canthi. Lacrimal gland the lacrimal gland is the first producer of the aqueous component of the tear layer. Tears are produced by the lacrimal gland and circulate inside the upper and decrease meniscus. Tears drain sequentially through the puncta, canaliculi, lacrimal sac and nasolacrimal duct. Acini consist of secretory cells that discharge their product into a central lumen steady with an intercalated duct fashioned from a single layer of epithelial cells that lack secretory granules. Myoepithelial cells lengthen processes across the perimeter of acini and ducts; their contraction imparts a mechanical pressure on the acini and ducts, which promotes the expulsion of tears from the gland. The interstices of the gland are composed of loose connective tissue that contains numerous immune cells, primarily B-lymphocytes and plasma cells (particularly IgA-secreting cells). The lacrimal gland consists of orbital and palpebral parts which are steady posterolaterally around the concave lateral edge of the aponeurosis of levator palpebrae superioris. The orbital part, about the size and shape of an almond, lodges in a shallow fossa on the medial side of the zygomatic process of the frontal bone, just inside the orbital margin. Its lower surface is related to the sheath of levator palpebrae superioris and its higher floor is related to the orbital periosteum. Its anterior border is in touch with the orbital septum and its posterior border attached to the orbital fats.
Forsythia Suspensa (Forsythia). Ponstel. - How does Forsythia work?
- What is Forsythia?
- Are there any interactions with medications?
- Are there safety concerns?
- Dosing considerations for Forsythia.
- Inflammation of small air passages in the lung (bronchiolitis), tonsillitis, pharyngitis, fever, gonorrhea, and inflammation.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97049
Order ponstel on line amexAfter a number of degrees of opening spasms in 7 month old purchase ponstel 500 mg mastercard, the condyle continues rotating inside its disc and muscle relaxant pills over the counter discount 250mg ponstel with visa, as properly as muscle relaxant intravenous generic ponstel 500 mg without prescription, each slide forwards down the articular eminence of the upper joint compartment muscle relaxant starting with z purchase genuine ponstel online. Without this ahead slide or translation, it turns into unimaginable to proceed opening the jaw beyond a gape of approximately 25 mm. When the jaw is rotated open, the temporomandibular ligament rapidly turns into taut (Osborn 1995). The taut ligament acts as a constraint that permits the mandible solely two rotary actions: it can swing about the higher attachment of the ligament and rotate in regards to the decrease attachment. The lower finish of the taut ligament acts as a transferring fulcrum that converts the downward and backward pull of the opening rotary drive (created on the front by digastric and geniohyoid) into one that drives the condyle upwards and forwards into the concavity of the overlying articular disc. Swing in regards to the higher attachment creates house above for the disc to slide additional forwards, which is possible as a outcome of the higher a part of the capsular ligament is unfastened. The two actions, rotation and swing, are inextricably linked by the taut ligament and, through the condyle, mix to hold the disc in firm contact with the articular eminence while the jaw is opened. The disc is stabilized by its tight attachment to the condyle (collateral ligament) and by the thickened margins of its anulus that prevent it sliding through the thinner compressed region between the centre of the condyle and the articular eminence. As forward slide of the condyle continues, the controlling affect exerted by the temporomandibular ligament diminishes. The lingula of the mandible strikes away from the spine of the sphenoid, tautening the initially slack sphenomandibular ligament, which now acts in the identical means as the temporomandibular ligament, to keep the condyle in opposition to the articular eminence. Symmetrical opening thus appears to include at least three separate phases: an early phase managed by the temporomandibular ligament and articular eminence; a brief middle phase during which either each temporomandibular and sphenomandibular ligaments, or neither, act to constrain actions; and a late section controlled by the sphenomandibular ligament and articular eminence. Key: 1, body of zygoma; 2, pterygopalatine fossa; three, temporalis; 4, lateral pterygoid; 5, condyle; 6, parapharyngeal fats stripe; 7, inside carotid artery; eight, jugular bulb/foramen; 9, coronoid process; 10, lateral pterygoid plate; eleven, torus tubarius; 12, fossa of Rosenm�ller; thirteen, longus colli; 14, exterior auditory meatus; 15, superficial lobe of parotid gland. The nerve supply to the temporomandibular joint is from branches from the mandibular division of the trigeminal nerve, largely by way of the auriculotemporal department, along with branches from the masseteric and deep temporal nerves. Postganglionic sympathetic nerves provide the tissues associated with the capsular ligament and the looser posterior bilaminar extension of the disc. The temporomandibular joint capsule, lateral ligament and retroarticular tissue include mechanoreceptors and nociceptors. The enter from mechanoreceptors offers a supply of proprioceptive sensation that helps control mandibular posture and motion. The joint derives its arterial provide from the superficial temporal artery laterally and the maxillary artery medially. Veins drain the anterior facet of the joint and related tissues into the plexus surrounding lateral pterygoid; posteriorly, they drain into the vascular region that separates the 2 laminae of the bilaminar region of the disc. Positive and unfavorable stress produced by forward and backward movement of the condyle shunts blood between these regions. Lymphatics drain deeply to the higher cervical lymph nodes surrounding the interior jugular vein. Humans use a lateral motion of the lower jaw to create a shear force that enhances the effectiveness of the facility stroke of mastication. Extensive lateral motion is only attainable when the jaw is rotated horizontally about one condyle whereas the opposite condyle slides backwards and forwards. The temporomandibular joint is structurally adapted to accommodate each sliding/translation and rotation/hinging in a sagittal airplane. This differential movement ends in the disc transferring solely about half the distance of the condyle. The adjustments in disc position could turn out to be out of phase with the condyle, inflicting obstruction to clean mandibular motion. The disc is often pulled anteromedially by the lateral pterygoid, so preventing ahead translation of the condyle. As the drive from the condyle on the disc increases, the elastic posterior attachments of the disc are stretched till the resistance to movement is overcome and the disc reduces into a normal relationship with the condyle, which is related to an audible click (audible to the affected person and infrequently to others). This phenomenon is called reciprocal clicking or disc displacement with reduction. This is a common medical situation and is known appropriately as closed lock or disc displacement with out discount (see below). Under these circumstances, jaw movements and the positions of the condyles are managed by neuromuscular processes (within the bounds of constraints imposed by the articular eminence, the occluding surfaces of the teeth and the presence of meals between them). Note that the non-working condyle strikes the furthest, and is probably the most heavily loaded, in the course of the power stroke of mastication.
Purchase ponstel mastercardThey are the buccal tissue space spasms 1983 youtube buy ponstel paypal, lying between the pores and skin and the floor of buccinator muscle relaxant neck generic 250 mg ponstel otc, and the infraorbital tissue space muscle relaxant homeopathy cheap ponstel 250mg online, lying between the bony attachments of levator labii superioris and levator anguli oris esophageal spasms xanax generic 500mg ponstel otc. The bones of the nasoethmoidal and zygomaticomaxil lary complexes are described right here. The external surface is convex and smooth, with a central parietal tuber (tuberosity). Curved superior and inferior temporal lines cross it and form posterosuperior arches. The temporal fascia is connected to the superior line or arch, and temporalis is attached to the inferior line or arch. The epicranial aponeurosis lies above these strains, and part of the temporal fossa lies below. Posteriorly, near the sagittal (superior) border, an inconstant parietal foramen transmits a vein from the su perior sagittal sinus and generally a department of the occipital artery. The inner floor is concave and marked by impressions of cere bral gyri and by grooves for the middle meningeal vessels. The latter ascend, inclining backwards, from the sphenoidal (anteroinferior) angle and posterior half (or more) of its inferior border. A groove for the superior sagittal sinus lies along the sagittal border and is completed by the groove on the opposite parietal bone. Granular foveolae for arachnoid granulations flank the sagittal sulcus and are most pronounced in old age. The dentated sagittal border, longest and thickest, articulates with the reverse parietal bone at the sagittal suture. The anterior part of the squamosal (inferior) border is brief, skinny and truncated, bevelled exter nally and overlapped by the larger wing of the sphenoid. It is type of separate from, and superficial to , the temporal fascia (deep temporal fascia). The plane between the temporoparietal fascia and the underlying deep temporal fascia contains loose areolar tissue and a small amount of fat. This tissue airplane, the temporoparietal fat pad, is continuous superiorly with the subgaleal plane of free areolar tissue within the scalp. Running superiorly within the temporoparietal fascia or simply deep to it are the superficial tem poral vessels, the auriculotemporal nerve and its branches, and the temporal branches of the facial nerve. When raising a bicoronal flap, identification of the temporoparietal fats pad helps to separate these two fascial layers; subsequent dissection in a plane deep to the temporo parietal fascia protects the temporal branch of the facial nerve. The 477 cHapTeR Retaining ligaments of the face 30 Parotid fascia (capsule) Buccinator is covered by a skinny layer of fascia, the buccopharyngeal fascia, which additionally covers the superior constrictor of the pharynx (Ch. The posterior part of the inferior border is short, thick and serrated for articulation with the mastoid half. The frontal border is deeply serrated, bevelled externally above and internally under, and articulates with the frontal bone to kind one half of the coronal suture. The occipital border, deeply dentated, articulates with the occipital bone, forming one half of the lambdoid suture. The frontal (anterosuperior) angle, which is roughly 90�, is at the bregma, where sagittal and coronal sutures meet, and marks the positioning of the anterior fontanelle within the neonatal skull. The sphenoidal (anteroinferior) angle lies between the frontal bone and higher wing of the sphenoid. Its internal floor is marked by a deep groove or canal that carries the frontal branches of the middle meningeal vessels. The frontal, parietal, sphenoid and temporal bones usually meet on the pterion, which marks the location of the sphenoidal fontanelle in the embry onic skull. The frontal bone generally meets the squamous part of the temporal bone, by which case the parietal bone fails to attain the larger wing of the sphenoid bone. The rounded occipital (posterosuperior) angle is on the lambda, the meeting of the sagittal and lambdoid sutures, which marks the site of the posterior fontanelle within the neonatal skull.
Buy ponstel cheap onlineFrom this region muscle spasms zyprexa purchase generic ponstel pills, the sturdy stylomandibular ligament ascends to the styloid course of infantile spasms 2013 purchase ponstel 250 mg without prescription. Inferiorly spasms left upper abdomen discount 250 mg ponstel with visa, along trapezius and sternocleidomastoid muscle relaxant 4211 v generic ponstel 250 mg otc, the invest ing layer of the deep cervical fascia is hooked up to the acromion, clavicle and manubrium sterni, fusing with their periostea. A quick distance above the manubrium, the investing layer interweaves with aponeurotic fibres of platysma and the fascia investing the strap muscular tissues. It is organ ized into superficial and deep layers, which are attached to the anterior border of the manubrium, and to the posterior border and the inter clavicular ligament, respectively. Between these two layers, a slitlike interval, the suprasternal space, accommodates a small quantity of areolar tissue, the lower elements of the anterior jugular veins and the jugular venous arch, the sternal heads of the sternocleidomastoid muscular tissues and generally a lymph node. It corresponds within the dwelling neck with the decrease a part of a deep, distinguished hollow, namely: the higher supraclavicular fossa. Its floor incorporates the primary rib, scalenus medius and the first slip of serratus anterior. Its size varies with the extent of the clavicular attachments of sternocleidomastoid and trapezius, and likewise the extent of the inferior stomach of omohyoid. The triangle is roofed by pores and skin, superficial and deep fasciae, and platysma, and crossed by the supraclavicular nerves. Just above the clavicle, the third part of the subclavian artery curves inferolaterally from the lateral margin of sca lenus anterior across the primary rib to the axilla. The brachial plexus is partly superior, and partly posterior, to the artery and is always intently related to it. The trunks of the brachial plexus might easily be palpated right here if the neck is contralaterally flexed and the examining finger is drawn throughout the trunks at proper angles to their size. With the musculature relaxed, pulsation of the subclavian artery may be felt and the arterial circulate may be managed by retroclavicular compression in opposition to the primary rib. The suprascapular vessels cross trans versely behind the clavicle, below the transverse cervical artery and vein. The exterior jugular vein descends behind the posterior border of ster nocleidomastoid to end in the subclavian vein. Other constructions throughout the triangle embody the nerve to subclavius, which crosses the triangle, and lymph nodes. Middle layer of deep cervical fascia Many of the variations in the descriptions of cervical fascia concern the middle layer. The visceral layer extends inferiorly from the base of the cranium posteriorly and the hyoid bone and thyroid cartilage anteriorly and laterally, and supplies fascial sheaths of varying thickness for the thyroid gland, larynx, trachea, pharynx and oesopha gus. Inferiorly, it continues into the superior mediastinum alongside the nice vessels and fuses with the fibrous pericardium. Deep layer of deep cervical fascia the deep layer of cervical fascia consists of dorsal and ventral layers: the prevertebral and alar fasciae, respectively. The prevertebral fascia lies closest to the vertebral bodies, covering the anterior surface of longus capitis and longus colli. It extends infer iorly from the skull base, descending in front of longus colli into the superior mediastinum, the place it blends with the anterior longitudinal ligament. It passes laterally and posteriorly as the scalene fascia, which covers the scalene muscle tissue, splenius capitis and levator scapulae. All the ventral rami of the cervical nerves are initially behind the prevertebral fascia. The nerves to the rhomboids and serratus anterior and the proxi mal parts of the phrenic nerve retain this position all through their course within the neck, however the accessory nerve lies superficial to the prever tebral fascia. As the subclavian artery and the brachial plexus emerge from behind scalenus anterior, they carry the prevertebral fascia down wards and laterally behind the clavicle because the axillary sheath. The pre vertebral fascia is connected to the spinous processes of the vertebrae and varieties a fascial flooring for the posterior triangle of the neck. The alar fascia is a coronally oriented sheet, connected to the trans verse means of the cervical vertebrae. It passes anterolaterally to fuse with the prevertebral fascia and extends inferiorly from the skull base to in regards to the degree of the seventh cervical vertebra (it varies between C6 and T4), where it fuses with the visceral layer of center cervical fascia, thereby delimiting the lowest extent of the retropharyngeal and danger areas. References:
|